How New Data is Helping Us Understand the Importance of Doctor Performance
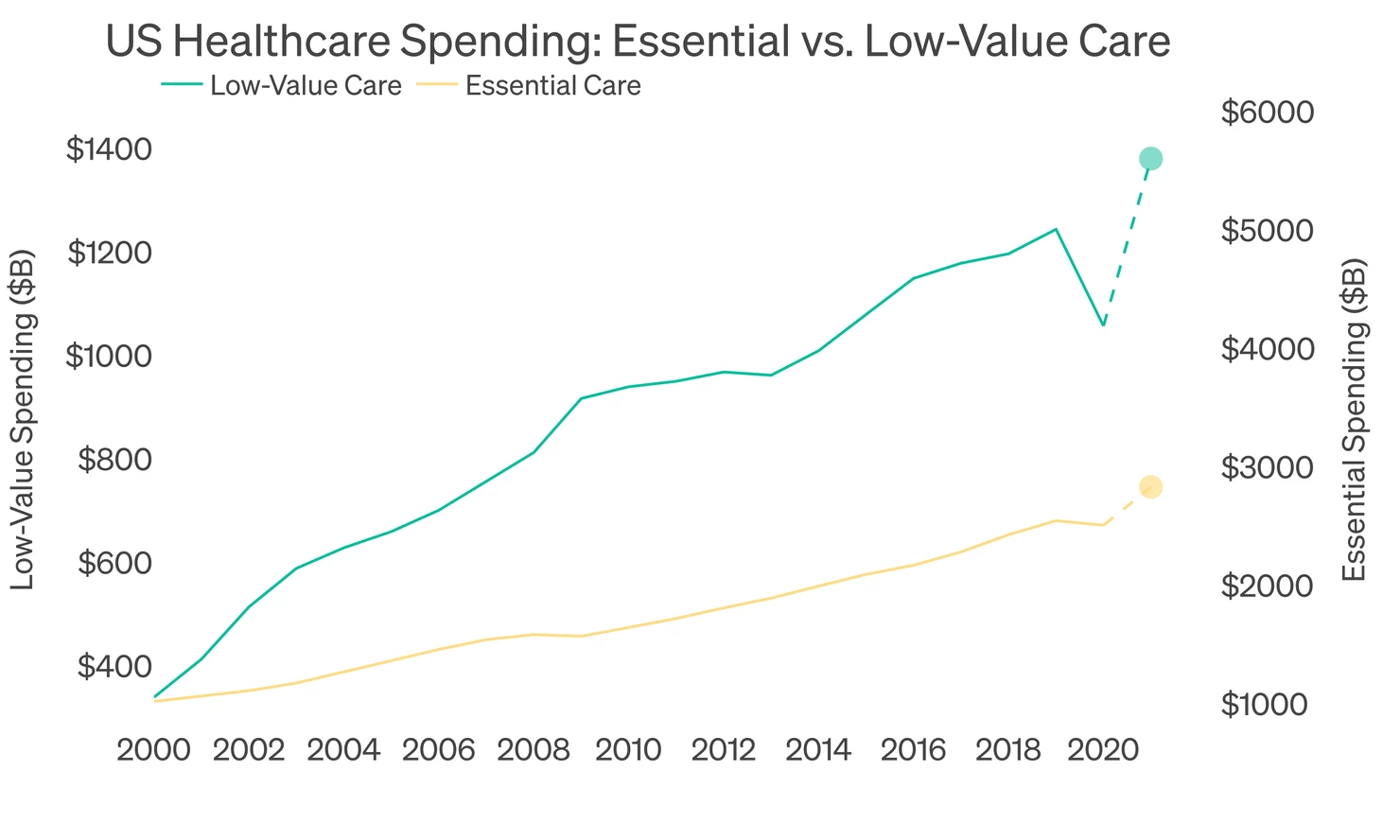
We believe this year will be a turning point for US employee health benefits: due to increased elective care after COVID, continued weakness in the economy and the ongoing bloat in the healthcare system, in 2021, for the first time ever, US companies will spend more on healthcare benefits than they make in profit [1]. In order to be successful, we believe most companies in the US will need to focus on their health plan operations just as much as they focus on their core business operations.
We have assembled over 45 billion claims records, giving us a unique opportunity to understand where the inefficiencies in the healthcare system come from and what to do about them. After analyzing this data, we believe the results are clear: the single biggest reason why healthcare costs are high is that many doctors fail to follow current medical best practice and also produce poor health outcomes. These failures to follow best practice and produce good outcomes (which we refer to as “low-value care”) cost a total of $1.4 trillion per year and cut 4 days from the healthy lifespan of a patient each time they use the healthcare system. In this report, we show the data that led us to these conclusions and describe how employers can improve their health plan’s performance by focusing on driving more care to the highest quality individual doctors in their community. To start, we show the total spending on “low-value care” which is the single fastest growing component of US healthcare spending.
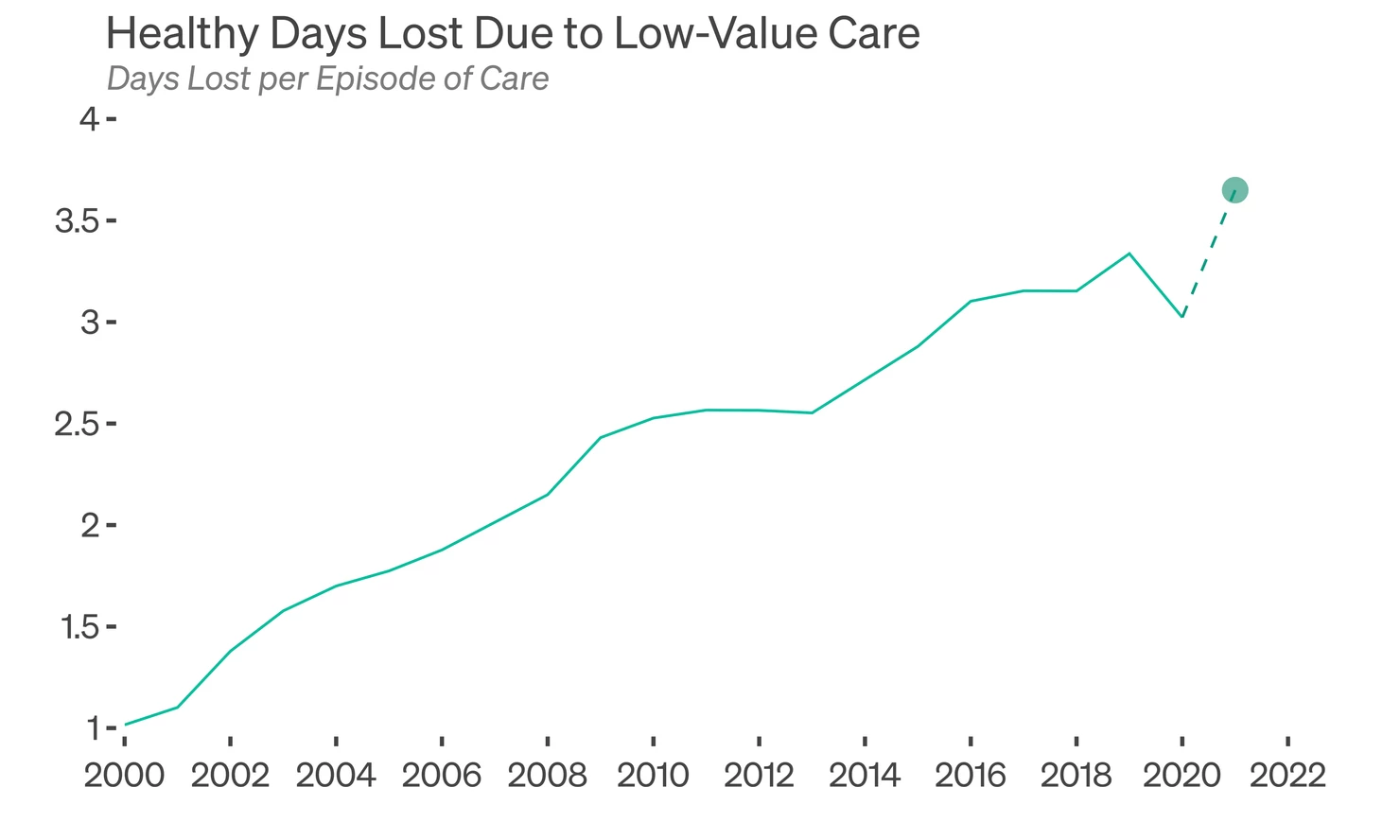
 Low-value care is not simply a cost issue: it also has a material impact on health outcomes. From observing hundreds of millions of patient journeys and reviewing hundreds of metrics on clinical best practice, we see that each year 44% of patients will receive a test or surgery that is not recommended by current best practice. These unnecessary procedures harm patients: unnecessary tests can lead to excessive surgical interventions, and unnecessary surgeries require recovery time and add risk of complications. We go claim-by-claim and calculate the number of days each patient loses from their healthy lives as a result of low-value care. We currently estimate that the average patient in the US loses nearly 4 days per episode of care.
Low-value care is not simply a cost issue: it also has a material impact on health outcomes. From observing hundreds of millions of patient journeys and reviewing hundreds of metrics on clinical best practice, we see that each year 44% of patients will receive a test or surgery that is not recommended by current best practice. These unnecessary procedures harm patients: unnecessary tests can lead to excessive surgical interventions, and unnecessary surgeries require recovery time and add risk of complications. We go claim-by-claim and calculate the number of days each patient loses from their healthy lives as a result of low-value care. We currently estimate that the average patient in the US loses nearly 4 days per episode of care.
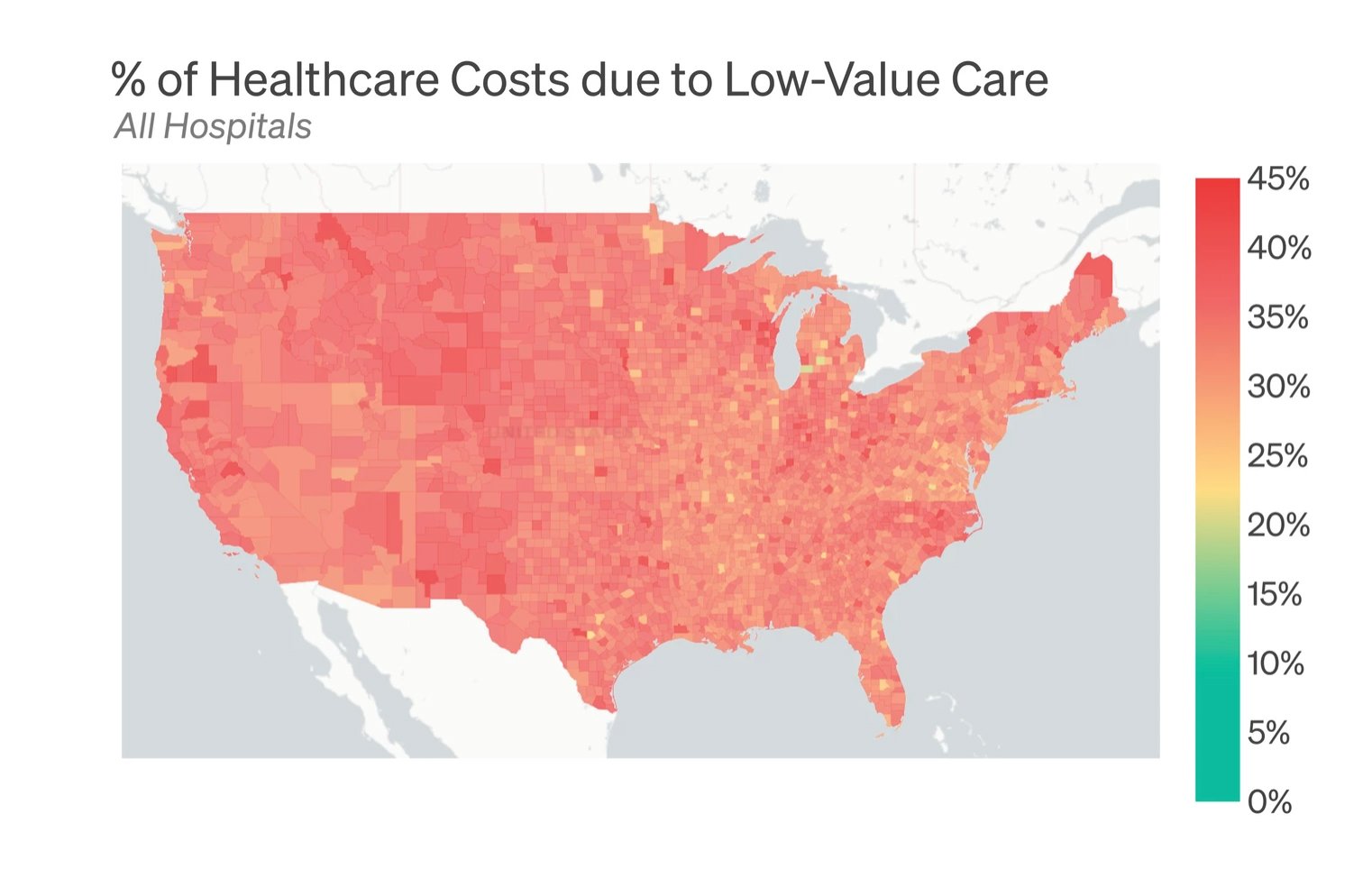
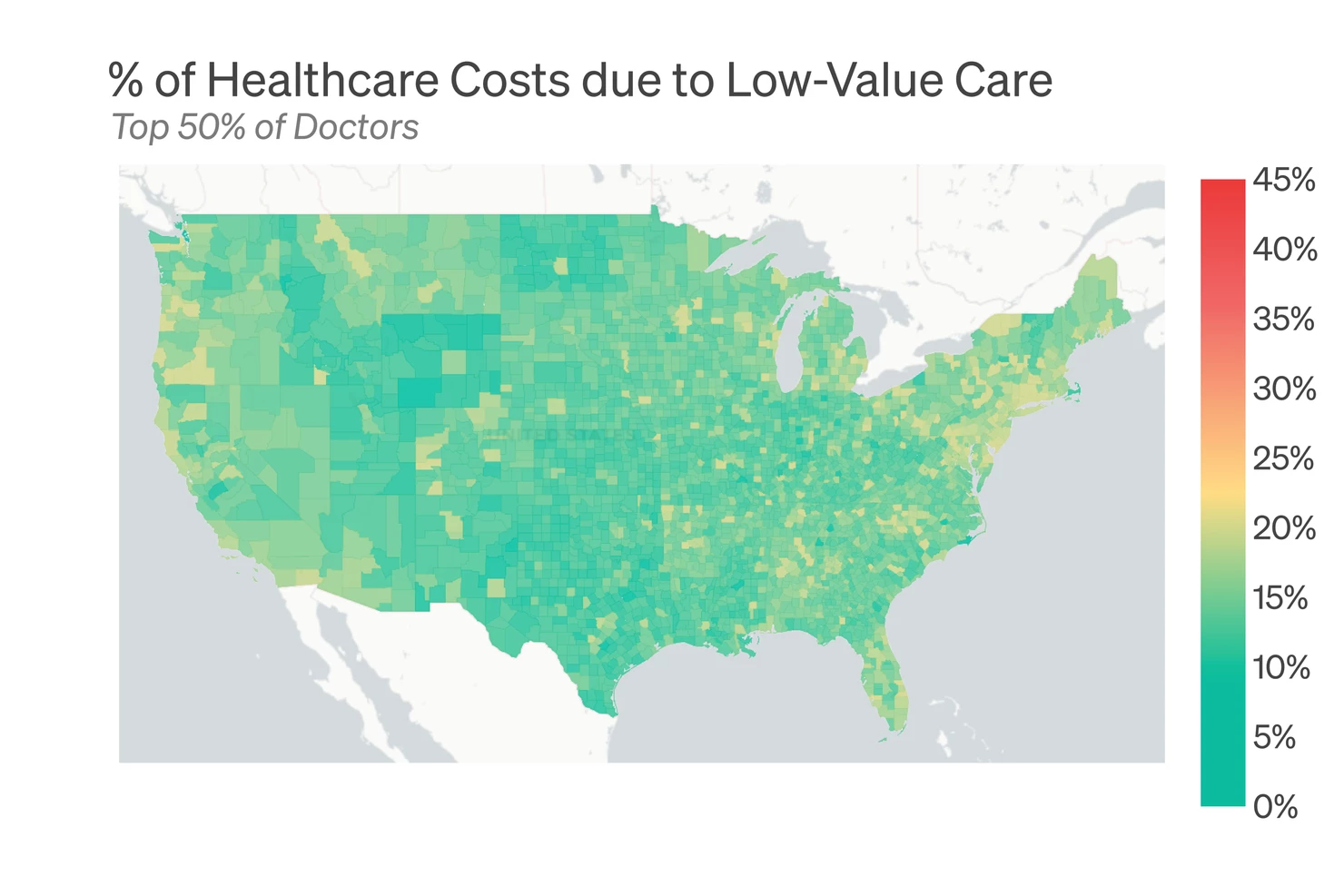
 Unfortunately, inappropriate care and bad health outcomes are pervasive in nearly every community in the country. The map below shows the percentage of costs that are due to low-value care throughout the US. As you can see, in almost every location, this care accounts for 30-40% or more of healthcare costs.
Unfortunately, inappropriate care and bad health outcomes are pervasive in nearly every community in the country. The map below shows the percentage of costs that are due to low-value care throughout the US. As you can see, in almost every location, this care accounts for 30-40% or more of healthcare costs.
 Traditional models have failed to improve low-value care
Traditional models have failed to improve low-value care
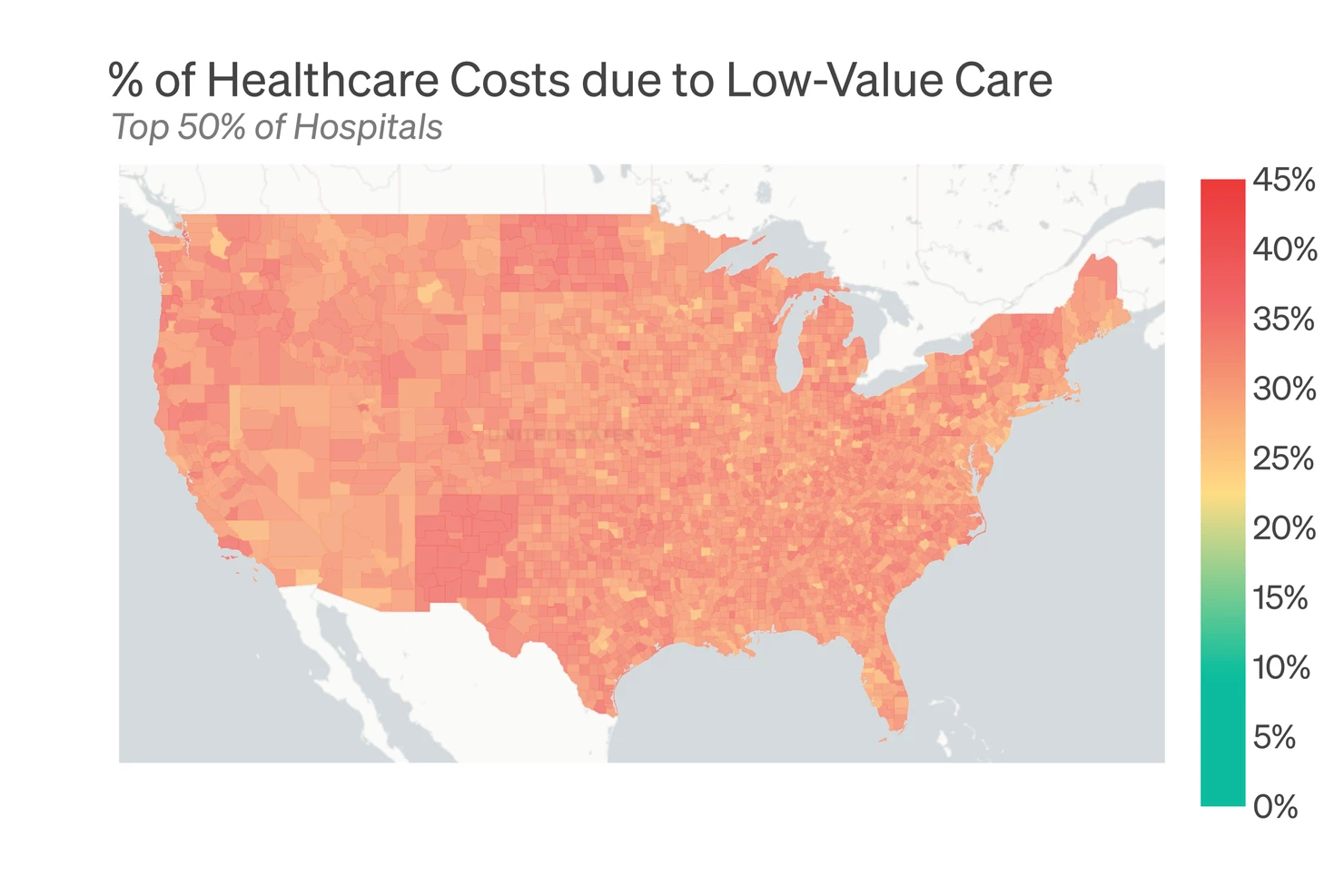
To date, much of the discussion around quality improvement has focused on “high performing” hospital networks. The idea has been to narrow the provider network to a select hospital system that lowers waste and improves quality. Unfortunately, these models have struggled to deliver real improvement. This is because most hospital systems either have no financial incentive to move towards high-value care (excess care adds to hospital revenues) or have struggled to change the clinical behaviors of their physicians. As one indication of the limited impact of “high performing” networks, below we show the same heat map of low-value healthcare if we only include the top 50% of best performing hospitals. The picture is only moderately improved.
 The key to improvement: doctor selection
The key to improvement: doctor selection
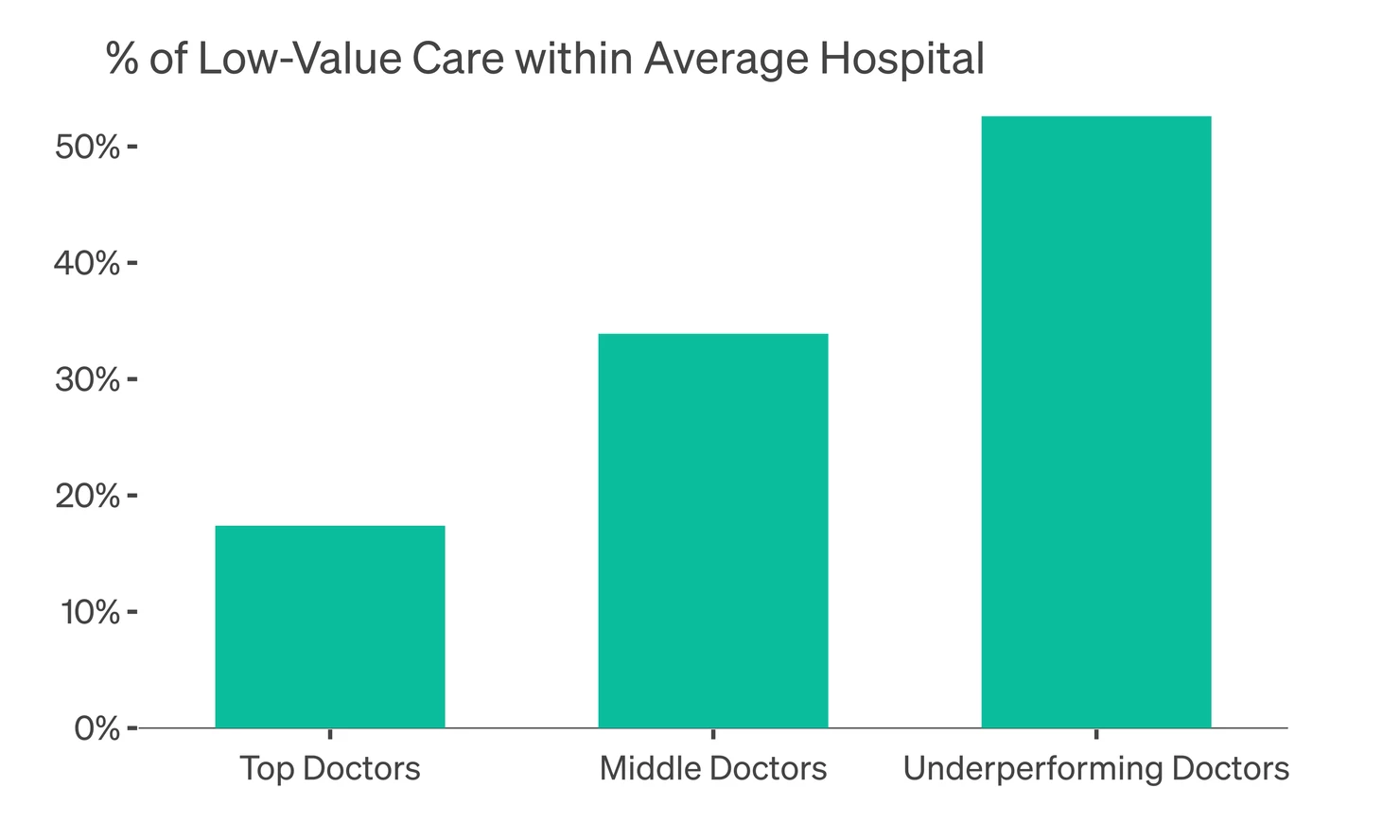
If high performing networks fail to meaningfully lower low-value care, how will employers create better outcomes for their health plans? Our extensive data analysis shows a clear silver lining: in every community in the country, there are high performing doctors who follow best practices and create excellent health outcomes for their patients. The data from these physicians is striking: if all patients saw top performing doctors the result would be 30% lower cost and 3 healthy days added to the life of every patient. To illustrate this, we looked into every hospital system in the country and segregated their physicians into three groups: “top doctors” (the top 25% of the hospital system in reducing low-value care), “underperforming” (the worst 25% in the hospital system at reducing low-value care) and “middle” (everyone else). What we found was striking: even within the same hospital systems there is a significant variation. Top doctors created 70% less low-value care as compared to their underperforming peers working at the same system.
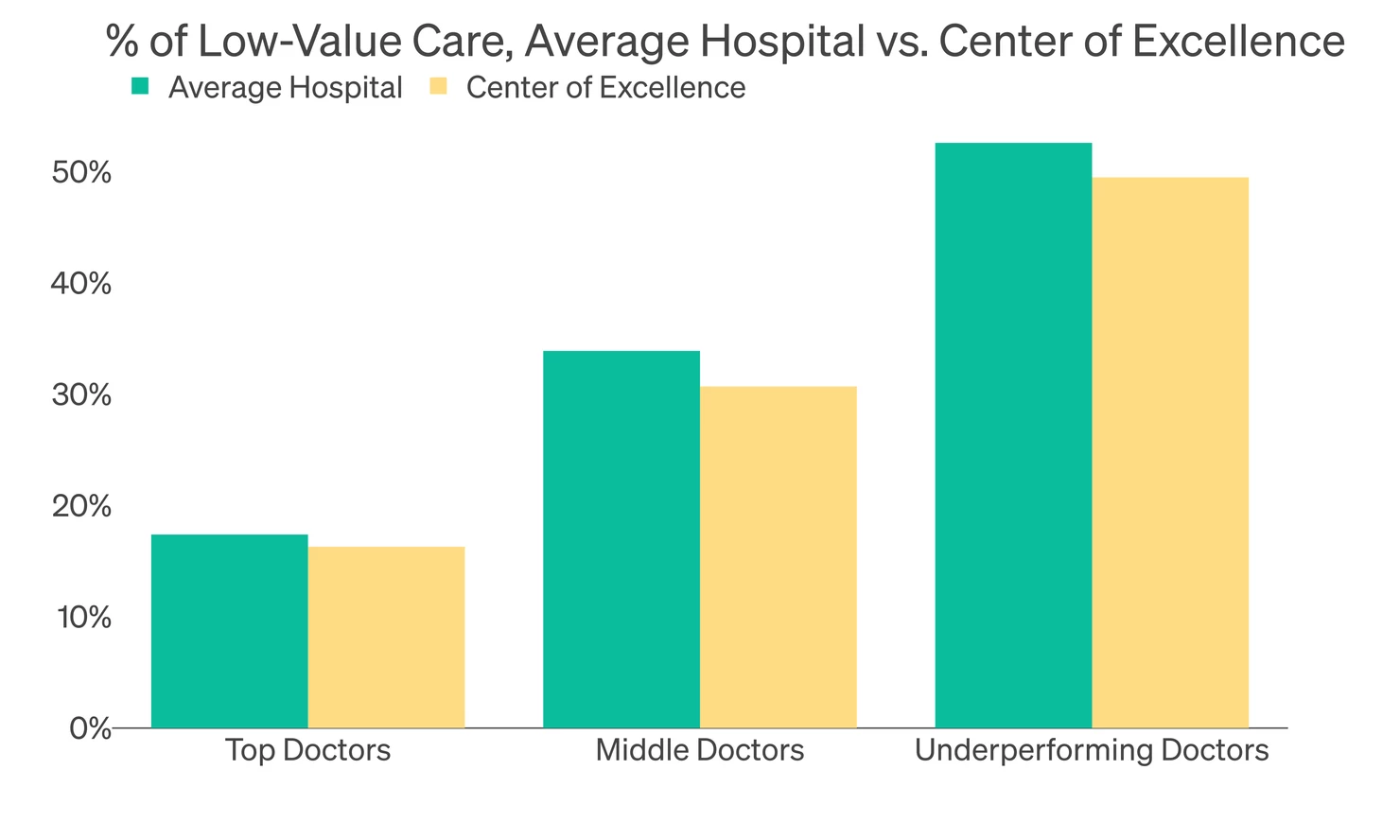
This variation in the quality of care is true in nearly every hospital system across the country. When we narrow the analysis to hospitals with great reputations that are commonly used as national “Centers of Excellence” we see the exact same picture: there is a large difference in quality between “top doctors” and “underperforming” doctors even at the best performing hospitals.
What if employers could get more care to these top performing doctors? To illustrate the impact, below we show the amount of low-value care when the map is narrowed to only the top 50% of all physicians. As you can see, nearly every community becomes a high-performing area. If all employees saw top performing doctors, we estimate the savings would be $2,100 per employee per year.
As we noted above, 2021 is likely to be a turning point as more employers focus on their healthcare benefits. We believe that if employers want to produce better health plan performance and cut low-value care, the key is identifying the best physicians in their local markets. If you have questions about how to manage low-value care in your local markets, feel free to contact us for a customized savings report.